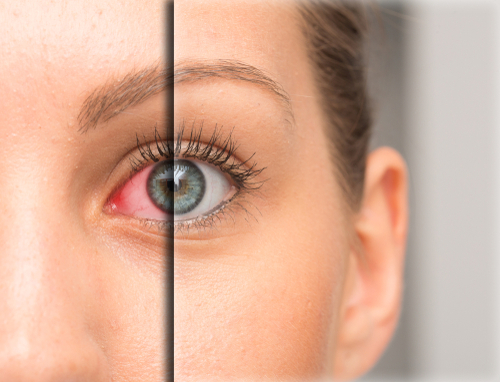
Your eyes may appear several different colors depending on a few factors: White, Red, Yellow, Blue, or Brown. Typically, those different colors are associated with certain systemic conditions.
White – Healthy and normal
Red - Infection, inflammation, injury, dryness, or a hemorrhage
Yellow – Jaundice
Blue - Thinning of the sclera (the white part of the eye), connective tissue disorders, certain medications, anemia, and a specific freckle called Nevus of Ota
Brown – Melanin, a freckle, or nerve bulbs called Axenfeld Loops
Let’s take a closer look at why your eyes might appear red.
Infection – Whether it’s viral, bacterial, or allergic, each of these will cause your eye to react in different manors but all will result in redness.
Viral infections sometimes need specific medications, even oral medications for treatment. Otherwise, they may be self-limiting, meaning your body needs to fight off the infection on its own. However, we can always help reduce the symptoms you’re experiencing with the use of eye drops.
Bacterial infections can range from mild to extremely aggressive. Some of those infections will resolve on their own with the help of your tear’s natural antibodies. Other more dangerous bacteria will require stronger and more specific antibiotic drops, sometimes even oral or IV medication.
Allergies, not quite the same infection as bacteria or a virus, but they can still cause redness, discharge, swelling, tearing, and itching. Treated with topical eye drops and oral allergy medications, most are available over the counter.
Inflammation – Sometimes the inflammation that occurs may be related to a systemic condition or simply isolated to the eye itself.
Iritis/Uveitis is inflammation of the eye that may cause redness, eye pain, light sensitivity and tearing. Typically, these are treated with dilation and steroid eye drops. Many times, this is linked to an underlying autoimmune disorder such as rheumatoid arthritis, IBS, ankylosis spondylitis, Sjogren’s, etc.
Episcleritis & Scleritis, both are inflammation of the white part of the eye, but episcleritis is more superficial, sometimes asymptomatic, and easier to treat. Scleritis is a deeper inflammation and causes severe, radiating eye pain and may even require hospitalization.
Pinguecula and Pterygium are benign growths on the white part of the eye and the cornea respectively. These gelatinous and fleshy growths are due in part to UV damage from the sun and excessive dryness from arid living conditions. This causes the surface to form a sort-of callus on the white part of the eye, called a pinguecula, or a fleshy growth on to the cornea, called a pterygium. Both conditions may become inflamed from time to time causing the eye to look redder. To prevent them from getting worse we recommend full UV protection with sunglasses when outdoors and artificial tears for lubrication.
Blepharitis, also known as inflammation of the eyelids, can cause a multitude of symptoms ranging from dryness to itching, and can even lead to lid and eye redness if left untreated.
Injury to the eye will normally cause redness. The body will respond by trying to bring a greater blood supply to the site of the injury which causes your blood vessels to dilate and engorge. This makes the eye look redder.
Dryness can cause many different symptoms but one of the hallmarks of dry eyes is redness. This happens when the eyes are not receiving enough tears, or the tears are evaporating too quickly. This causes the eyes to become inflamed as the cornea begins to dry out and starts getting irritated.
Hemorrhage of the subconjunctival space (between the clear and white layers of the eye) can happen for several different reasons, but the most common are:
Stress
Hypertension
Diabetes
Blood clotting disorders
Lifting something heavy
Rubbing your eyes
Injury
Straining
Blood thinners
Most of these hemorrhages will resolve on their own, just like a bruise, and the resolution time varies depending on the size and root cause of the hemorrhage. If you are experiencing multiple episodes of subconjunctival hemorrhages consult with your optometrist and primary care physician for further investigation.
If you simply want your eyes to temporarily look less red, I recommend Lumify by Bausch and Lomb, it works in 1 minute and lasts about 8 hours. I would NEVER use other products like Clear Eyes, Visine, and Rhoto. They contain ingredients such as tetrahydrozoline and naphazoline which are vasoconstrictors. They make the eyes look less red by constricting the blood vessels in the eye, after that they “re-dilate” to a larger size than their original state, known as the “rebound effect”, thus making the eyes look redder than when they started. So you use another drop… and another, and another, and another. Before you know it, you’re already on your second bottle. Do you see the pattern? The important thing is to treat what is causing the redness, not simply getting the red out. Otherwise, you’re wasting your time and money, and possibly hurting your eyes.
As you can see there are a variety of different reasons your eyes may look red. Occasionally it’s something simple that will go away on its own and other times you may require specific treatment. It’s always best to get things looked at by an eye doctor to properly diagnose the issue.